“Txin achigalix anĝaĝigumin anuxtanatxin ax̂saasaduukux̂tin. / Huzugaan txin achigax̂agacha mada ama txin sakaaĝatada.”
“Always learn and maintain a balance.”
– Unangan/Unangas value11
Last updated April 2021
What is Birth Control?
Birth control, also known as contraception, is any method, medicine or device used to prevent unplanned pregnancy. There are many types of birth control, which can be categorized by level of effectiveness at preventing pregnancy:
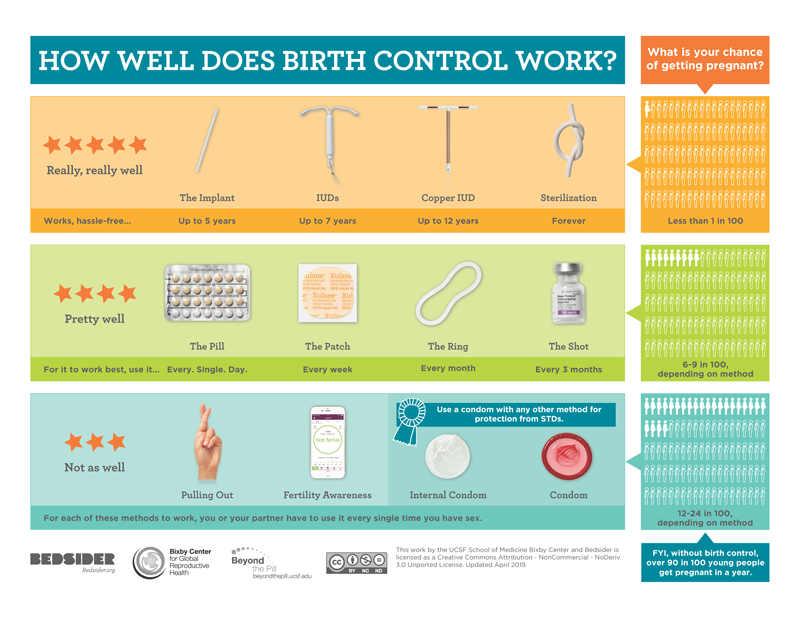
While the main use of birth control is to prevent pregnancy, there are also some other health benefits to taking birth control. Some forms of birth control, like condoms, can help protect against sexually transmitted infections (STIs) and diseases (STDs) . Other forms of birth control, like hormonal birth control, can help to regulate periods, reduce acne or even reduce pain from medical conditions like endometriosis.
There are many types of birth control, which we will explore below. The best form of birth control is one that is selected with a health care provider. Sometimes this is through trial and error, where a person will try various forms of birth control to find what is right for them.
When deciding which form of birth control is the right fit for any person, it is important to consider:
What Are the Different Kinds of Birth Control?
We’ll list the categories of birth control by the way they reduce the user’s risk for unplanned pregnancy. These methods include:
- Barrier methods
- Short-acting hormonal methods
- Long-acting methods
- Self-awareness methods
- Emergency contraception
Barrier Methods
Barrier methods help keep sperm from physically reaching the egg through the use of a safer sex tool. Barrier methods typically don’t involve hormones, and are considered to be short-term birth control. This means that barrier method condoms need to be removed after each use. Some barrier methods like condoms, spermicide or the sponge, are easily available at places like clinics, online shopping, or even at drug stores. Other barrier methods may require a prescription from a provider, like diaphragms or cervical caps.
Short-acting Hormonal Methods
Short-acting hormonal methods reduce the user’s risk for pregnancy by stopping the ovulation and fertilization of the egg, but do not protect against STIs. These methods work by increasing the production of a certain type of hormone made in the body. These are considered to be ‘short-acting,’ which means that the user has to take this form of birth control on a very regular basis, like daily, weekly, or monthly. It might help to use a birth control reminder app, or phone reminders, to keep track of when to take a short-acting hormonal birth control. Stopping the use of a short-acting hormonal method of birth control may greatly increase a person’s risk for pregnancy if another method is not used, like a condom.
Long-acting Contraceptive
Long-acting contraceptives reduce the user’s risk for pregnancy in different ways, but do not protect against STIs. Some of these methods work by increasing the production of a certain type of hormone made in the body. Others work through the use of non-hormonal intervention. These are considered to be ‘long-acting,’ which means that the user only has to monitor this form of birth control in their body once every few years, as directed by their health care provider. Although the provider may offer reminders of when it is time to switch-out the use of a long-acting reversible contraceptive, it might help to use a birth control reminder app, or phone reminders.
Self-awareness Methods
There are other forms of contraceptives that do not involve outside intervention, prescriptions, hormones, or safer sex tools. These methods of birth control do not protect against STIs.
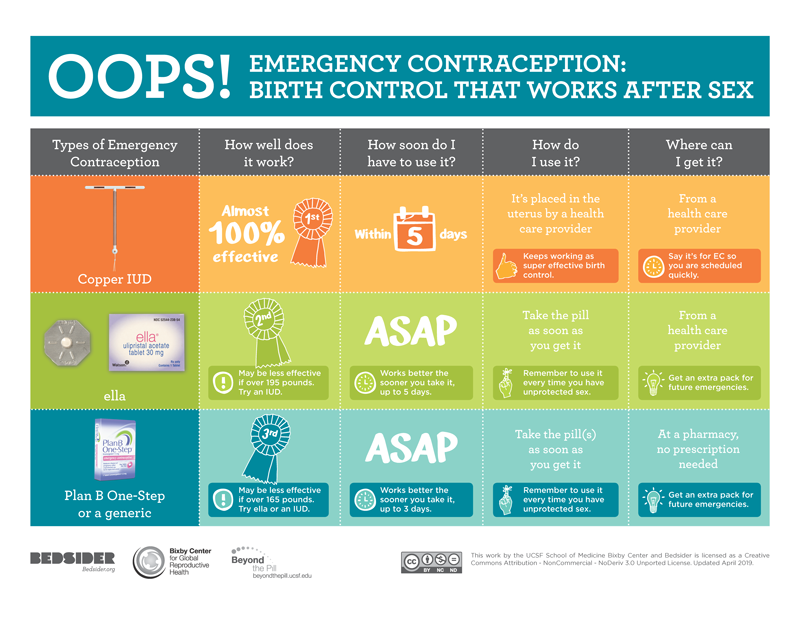
Emergency Contraception
Emergency contraception is used when individuals have unprotected sex, or if a used birth control method fails. Emergency contraception doesn’t protect against STIs, but it helps to reduce the user’s risk of pregnancy if taken up to three to five days after unprotected sex. There are both hormonal and non-hormonal types of emergency contraception.
Where Can I Go for More Information on Birth Control?
To learn more about birth control options and to receive guidance on which method is best for a person’s unique situation, consider speaking to a local health care provider or a trusted adult.
- Find a local health care provider in Alaska for more information
- Alaskans may order condoms from the iknowmine store, for free, sent right to your home in a discrete package! Non-profit and Tribal Organization orders are welcome, and available in bulk.
- Take a look at We R Native’s very own Auntie Amanda’s response to the question ‘What is the best birth control?’
- Resource for Parents and Caring Adults: Join Talking is Power, a weekly text messaging series for parents and caring adults. We know talking to teens about sensitive topics is never easy, but it’s important to talk to them openly and honestly. Text the word “EMPOWER” to 97779 and you’ll receive culturally appropriate tips and resources, covering sexual health, pregnancy, STDs and consent!

